Lancet:舒尼替尼和索拉非尼治疗肾癌有效性较差
2016-03-09 崔倩 译 MedSci原创
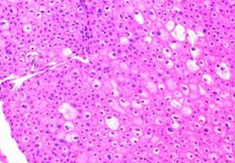
肾细胞癌是具有高血管密度的,并主要通过血管内皮生长因子(VEGF)通路的失调增殖。研究人员在切除局部疾病并具有复发高风险的患者中,测试了舒尼替尼和索拉非尼,两种口服抗血管生成剂,对于晚期肾细胞癌的有效性。原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Lancet#
52
可见目前不适用辅助治疗
169
主要目的是在意向治疗人群中比较每个实验组和安慰剂组之间的无病生存
147
符合条件的患者病理分期为高级T1b或更高,具有完全切除非转移性肾细胞癌
137
双盲、安慰剂对照、随机、3期试验
143
这和癌症类型相关吗
173
一个是辉瑞,一个是拜耳
60