Stroke:三甲胺氮氧化物与卒中复发的关系取决于缺血性卒中亚型
2021-11-21 MedSci原创 MedSci原创
TMAO水平升高与小动脉闭塞亚型患者卒中复发风险增加相关,但这种关联似乎在大动脉粥样硬化、心源性栓塞和其他亚型中有所减弱。
三甲胺N-氧化物(TMAO)已被公认为是心血管疾病的危险因素。然而,TMAO在缺血性卒中中的作用尚未明确。众所周知,缺血性脑卒中是一种发病机制多样的异质性疾病。近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在根据病因亚型研究TMAO与卒中复发之间的关联。

该研究共纳入了第三届中国卒中登记中心的10756例缺血性卒中/短暂性脑缺血发作患者,研究人员分析了卒中复发的1年随访资料。TOAST(急性中风治疗中的ORG10172试验)标准用于对病因亚型进行分类。受试者血浆TMAO水平是通过液相色谱-质谱法进行定量。研究人员使用Cox回归模型分析了TMAO与卒中结局之间的关联,研究人员还对TMAO水平与卒中风险的关联进行了荟萃分析。
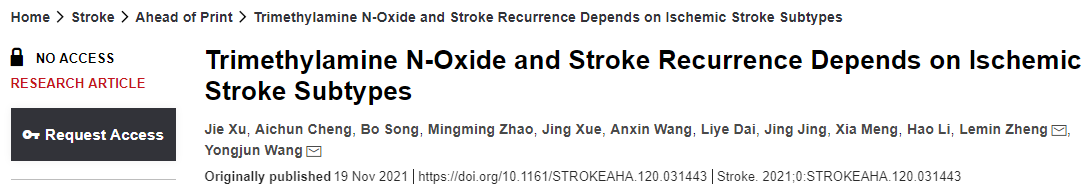
在多变量Cox回归模型中,TMAO水平升高与卒中复发风险独立相关(Q4与Q1:调整后的风险比为1.37[95%CI为1.15-1.64])。
按TOAST亚型分层后,TMAO与小动脉闭塞亚型的卒中复发之间存在显著关联(调整风险比为1.43[95%CI为1.03-2.00]),但在其他亚型(大动脉粥样硬化为1.19[0.95-1.48];心源性栓塞为1.54[0.95-2.48];其他为1.19[0.98-1.44])。荟萃分析报告了最高与最低TMAO水平的卒中复发汇总风险比为1.66(95%CI为0.91-3.01),同样发现卒中复发风险增加。
由此可见,TMAO水平升高与小动脉闭塞亚型患者卒中复发风险增加相关,但这种关联似乎在大动脉粥样硬化、心源性栓塞和其他亚型中有所减弱。
原始出处:
Jie Xu.et al.Trimethylamine N-Oxide and Stroke Recurrence Depends on Ischemic Stroke Subtypes.stroke.2021.https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.031443
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#卒中亚型#
73
#缺血性卒#
100
#缺血性#
0
#卒中复发#
109
#三甲#
101