Am J Pathol:抗生素的副作用:影响青春期后的骨骼发育
2019-01-20 佚名 中国生物技术网
众所周知,肠道菌群对我人体健康至关重要,大多数时候,我们都能与它们和谐共处。肠道微生物组调节我们的一系列生物功能,其中包括骨骼健康。
众所周知,肠道菌群对我人体健康至关重要,大多数时候,我们都能与它们和谐共处。肠道微生物组调节我们的一系列生物功能,其中包括骨骼健康。
如何维持肠道菌群的平衡呢?在健康饮食之外,很多人都知道抗生素不能过多服用的道理。因为抗生素滥用不仅会让病菌产生耐药性,还容易杀死肠道中的有益菌,带来健康隐患。
近日,美国南卡罗莱纳医科大学(MUSC)骨骼免疫学的研究人员发现抗生素会破坏健康肠道微生物组对青春期后骨骼发育的影响。该研究结果于2019年1月16日发表在《American Journal of Pathology》上,表明抗生素破坏肠道微生物群会诱导促炎反应,导致破骨细胞活性增加。
研究通讯作者、助理教授Chad M. Novince博士从事微生物对骨骼免疫和骨骼发育影响的研究,他说:“抗生素作为青春期后骨骼发育过程中肠道菌群骨免疫反应的关键外源性调节剂。已有研究证明抗生素会扰乱微生物组,但这是第一次评估抗生素对调节骨细胞和整体骨骼表型的免疫细胞下游影响的研究。这项工作将整个“故事”融合在了一起。”
青春期后的发育阶段是可塑性的关键时期,支撑着大约40%的峰值骨量。Novince实验室最近的研究表明,肠道微生物组有助于骨骼健康。为了确定抗生素干扰肠道菌群对青春期后骨骼发育的影响,Novince与包括微生物学家Alexander V. Alekseyenko博士在内的MUSC研究团队合作。他们使用三种抗生素混合物对小鼠进行治疗后发现,抗生素导致肠道微生物发生重要改变,引起多种细菌发生特殊变化。Novince说:“Alekseyenko博士的加入对于团队来说是巨大的助力。”
在小鼠的肠道菌群被抗生素破坏后,Novince的实验室测试了它们骨骼系统的完整性。抗生素诱导的肠道菌群变化对皮质骨的影响很小,然而,骨小梁却发生了明显变化,其骨质类型经历了高骨代谢率。虽然过去的研究关注了抗生素治疗对整体骨骼中骨细胞密度的影响,但是该研究集中在骨骼维持的细胞细节。骨代谢受骨再吸收(破骨细胞)和骨形成(成骨细胞)之间的平衡来控制。有趣的是,成骨细胞没有变化,而破骨细胞的数量、体积和活性都增加了。
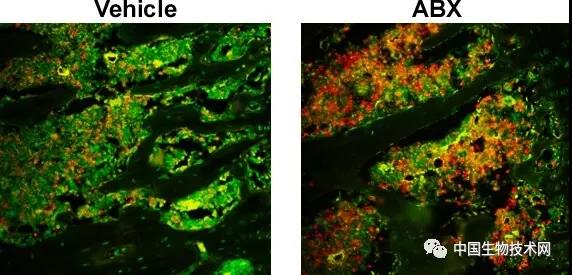
与对照组小鼠(左侧)相比,接受抗生素治疗的小鼠(右侧)导致骨髓MDSC细胞增加。图片来源: Dr. Chad Novince of the Medical University of South Carolina
为了确定导致破骨细胞活性增加的原因,Novince评估了几种破骨细胞信号分子的水平。他们发现,在接受抗生素治疗动物的循环系统中,促进破骨作用的信号分子水平增加,这表明破骨细胞活性增加的原因是机体对微生物组变化的特异性免疫反应的结果。
接下来的主要问题是,抗生素如何影响骨髓环境中的免疫细胞。
该研究第一作者Jessica D. Hathaway-Schrader博士说:“我们的研究实际上能够深入骨髓环境中特定的适应性和先天免疫细胞机制,从而证明这对骨髓细胞有影响。。”
通过对骨髓中的免疫细胞群进行分析,他们惊讶地发现在接受抗生素治疗的小鼠体内髓源性抑制细胞(MDSC)显着增加。已知MDSC在各种疾病期间调节先天性和适应性免疫应答,但尚未在健康方面进行广泛研究。此外,抗生素治疗抑制了抗原在骨髓中的表达和处理。
总而言之,Novince的团队发现,被抗生素扰乱的肠道菌群会导致免疫细胞与骨细胞之间的通信异常。虽然这项研究使用了广谱抗生素混合物来破坏肠道细菌的组成,但这些结果值得进一步研究。未来的研究目标是找到更适合人类的抗生素疗法。
Novince说:“我们还应该进行临床试验,以确定特定抗生素对肠道微生物组的影响。这项研究将支持开发靶向微生物组的预防和治疗骨骼恶化的非侵入性治疗干预措施。”
原始出处:Jessica D. Hathaway-Schrader, Heidi M. Steinkamp, Michael B. Chavez, et al. Antibiotic Perturbation of Gut Microbiota Dysregulates Osteoimmune Cross Talk in Postpubertal Skeletal Development. Am J Pathol. February 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#副作用#
64
#Pathol#
62
#青春期#
55
#发育#
57
严格掌握抗生素的使用。
96