右心房压力或许代表左心疾病引起的肺动脉高压的累计心脏负担
2022-02-18 刘少飞 MedSci原创
一些心力衰竭 (HF) 和射血分数保留 (HFpEF) 患者的右侧充盈压升高。我们假设右心房压力 (RAP) 代表左心、肺血管和右心异常的累积负担。
超过一半的心力衰竭 (HF) 患者具有左心室 (LV) 保留射血分数 (HFpEF)。继发于 LV 舒张功能障碍的左心充盈压升高是 HFpEF 患者的基本异常。LV 充盈压升高与不良临床结果相关,无论是通过侵入性测量的肺毛细血管楔压 (PCWP) 还是使用多普勒超声心动图的非侵入性估计来评估。
一些 HFpEF 患者的右侧充盈压也升高。HFpEF 中右心充盈压升高可能由肺动脉高压 (PH) 介导,这是由于高 LV 充盈压、右心室 (RV) 功能障碍、三尖瓣关闭不全恶化、右心房 (RA) 功能障碍和心房颤动负担增加所致(AF),每一个都与不良结果相关。因此,我们推测右侧充盈压可能代表这些心脏异常的累积负担,并可能为 HFpEF 的风险分层提供有价值的信息。使用基于下腔静脉 (IVC) 形态的超声心动图可以很容易地估计右心充盈压,但很少有研究报告估计的右心房压力 (eRAP) 对 HFpEF 患者的预后价值。因此,本研究的目的是调查 eRAP 与 HFpEF 患者临床结果之间的关系,并评估 eRAP 与其他指示左心、肺血管和右心异常的超声心动图标志物之间可能存在的等级关系。
研究方法及人群:
在这项回顾性观察性研究中,我们评估了 RAP 超声心动图标志物与 HFpEF 稳定患者临床结果之间的关联。本研究的一些参与者数据之前已发表,但与 eRAP 的预后价值无关。我们确定了 2014 年 1 月至 2019 年 6 月期间在日本前桥市群马大学医院或 2014 年 1 月至 2018 年 12 月期间在日本札幌北海道大学医院收治的患者。HFpEF 的诊断被定义为 HF 的典型临床症状(劳累性呼吸困难、疲劳或外周水肿),EF ≥ 50%,并且至少有以下一项:直接测量的 PCWP > 15 mmHg,B 型利钠肽 (BNP) 水平 > 200 pg/mL,比率舒张早期二尖瓣流入速度与舒张早期二尖瓣环组织速度 (E/e') > 15,左心房 (LA) 容积指数 > 34 mL/m 2或先前因 HF 相关的住院。
研究结果:
基线特征显示本研究共有 399 名 HFpEF 患者符合该研究的纳入标准。正如预期的那样,eRAP 为 15 mmHg 的患者右心重构和功能障碍最严重,但 eRAP 为 8 mmHg 的患者显示出更大的 LV 质量指数和 LA 体积指数、更高的 eRVSP、更大的 RV 和 RA 大小,以及更高的显着 TR 患病率(≥中度)比 eRAP 为 3 mmHg 的患者。鉴于 eRAP 为 8 mmHg 的 HFpEF 患者存在心脏重构和功能障碍,参与者根据 eRAP 分为两组:正常 eRAP(eRAP 为 3 mmHg)和较高的 eRAP(eRAP ≥ 8 mmHg)。
心脏重塑和功能障碍的比较
与 eRAP 正常的受试者相比,eRAP 较高的受试者显示出较大的 LV 质量指数和舒张末期容积,而各组之间的 EF、二尖瓣速度和 CO 相似。较高 eRAP 组患者的二尖瓣 E 波和 LA 体积指数大于正常组,表明左室舒张功能较差。高 eRAP 组中度二尖瓣反流的发生率高于正常 eRAP 组。正如预期的那样,eRAP 较高的患者的右心结构和功能异常比 eRAP 正常的患者更严重,包括较高的 eRVSP、较低的 TAPSE、较大的 RV 直径和 RA 体积指数,以及中度或重度 TR 的患病率较高。
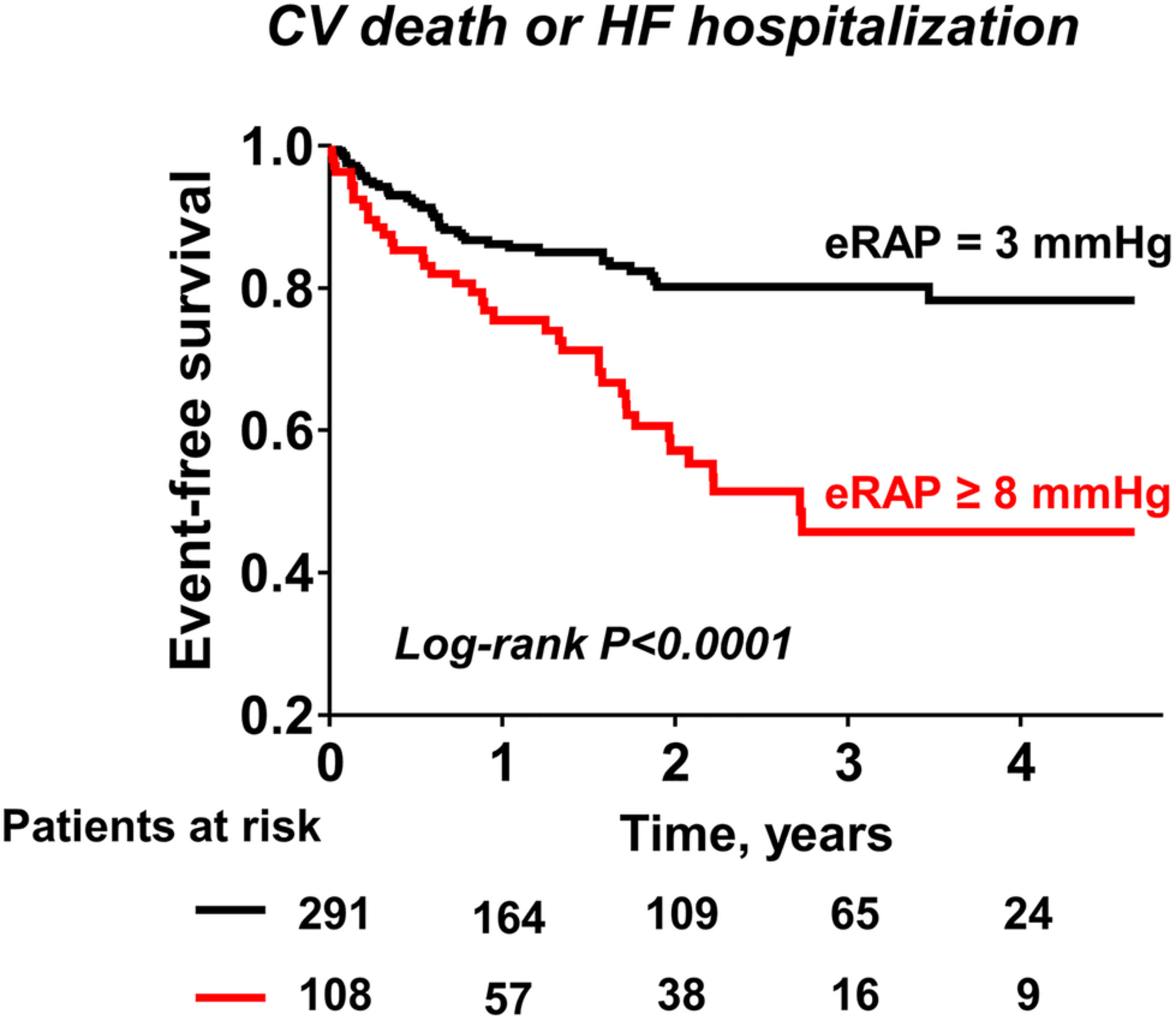
Kaplan-Meier 曲线分析表明,与 eRAP 正常的患者相比,eRAP 较高的患者心血管死亡或心衰住院的综合事件发生率较高(图 )。在单变量 Cox 比例风险模型中,与正常 eRAP 相比,eRAP ≥ 8 mmHg 的不良结局风险增加超过两倍。年龄、房颤的存在、利尿剂的使用、BNP 水平、LA 体积指数、E/e' 比、eRVSP、TAPSE、RV 中腔直径和 RA 体积指数也与事件终点相关。在一项多变量分析中,在调整了年龄、AF、利尿剂、BNP、E/e' 比、TAPSE 和 RV 中径后,较高 eRAP 的存在仍然与不良结局独立相关。
研究结论:
较高的 eRAP 与复合结局的风险增加独立相关,其预后价值超过 E/e' 比。我们还证明,eRAP ≥ 8 mmHg 是结果的最强预测因子,其次是 RV 中径、E/e' 比和 eRVSP,对患者的风险进行分层。我们的数据可能为 RA 高血压在 HFpEF 复杂病理生理学中的预后作用提供新的见解,并提示 eRAP 的预后效用。
参考文献:
Nagata R. Right atrial pressure represents cumulative cardiac burden in heart failure with preserved ejection fraction. ESC Heart Fail. 2022 Feb 15. doi: 10.1002/ehf2.13853. Epub ahead of print. PMID: 35166056.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
57
#右心房压力#
81
#右心房#
91
#心房#
87
不错,学习了。
67
学习了。
81
学习一下
70
不错学习了
71