Wnt信号通路指导的抗癌治疗
2015-10-10 Eason/编译 生命奥秘
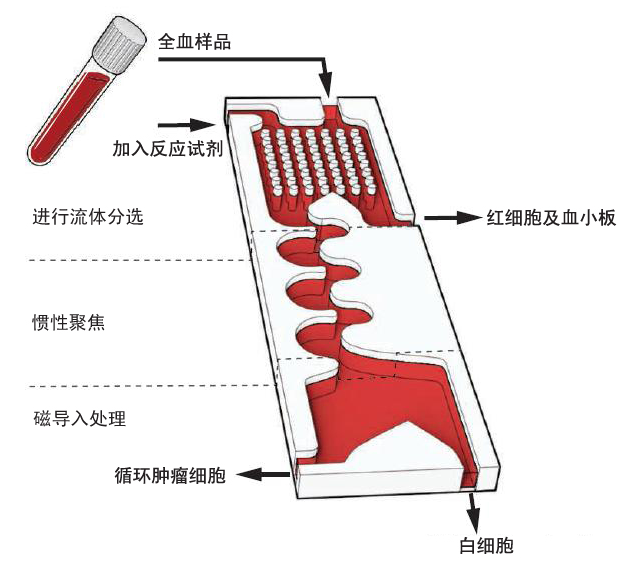
Wnt信号通路可能是让前列腺癌细胞得以逃避雄性激素受体抗癌靶向药物攻击的原因。能够从肿瘤患者体内分离得到循环肿瘤细胞(circulating tumor cells, CTC),并且对其进行鉴定的新技术让靶向抗癌治疗成为了可能,这对前列腺癌转移(metastatic prostate cancer)患者更加具有吸引力。这种患者通常都在几年前就做了原发灶切除手术,然后我们就只能够通过观察他们血液
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Wnt信号#
85
#Wnt信号通路#
73
#抗癌治疗#
94
#信号通路#
0
#WNT#
63
感谢作者分享
123