Lancet oncol:3期| 术前短疗程放疗+化疗可改善局部晚期直肠癌患者预后
2020-12-10 MedSci原创 MedSci原创
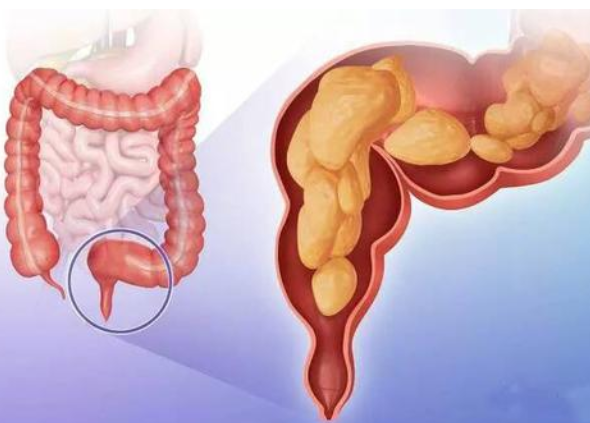
全身复发仍然是局部晚期直肠癌的主要问题。RAPIDO试验旨在评估短疗程放疗继以化疗和延迟手术对晚期直肠癌远处转移风险的控制效果。
全身复发仍然是局部晚期直肠癌的主要问题。RAPIDO试验旨在评估短疗程放疗继以化疗和延迟手术对晚期直肠癌远处转移风险的控制效果。
该试验是一项多中心、开放标签、随机对照的3期试验,从多个国家的54个中心招募年满18岁的活检确诊的原发局部晚期直肠腺癌患者。1:1将受试患者随机分至两组,实验组患者接受短疗程放疗(5×5 Gy,不超过8天)→6个疗程的CAPOX化疗(卡铂、奥沙利铂)或9个疗程的FOLFOX4(奥沙利铂、亚叶酸、大剂量氟尿嘧啶)→全直肠系膜切除;标准治疗组患者接受28×1.8 Gy或25×2 Gy放疗,同时每天口服卡铂,然后手术。主要终点是3年疾病相关治疗失败,包括局部衰竭、远处转移、新的原发结直肠肿瘤或治疗相关死亡。
2011年6月21日-2016年6月2日,共招募了920位患者,其中912位符合要求(实验组 462位、标准治疗组 450位)。中位随访4.6年(IQR 3.5-5.5)。随机分组3年后,实验组和标准治疗组的疾病相关治疗失败的累积发生率分别为23.7%(95% CI 19.8-27.6)vs 30.4%(26.1-34.6;风险比[HR] 0.75%,95% CI 0.60-0.95,p=0.019)。
手术前的最常见的3级及以上副作用是腹泻(实验组 81例[18%] vs 标准组 41例[9%]),辅助化疗期间的是神经毒性(标准组 16例[9%])。重度不良反应见于实验组的177位患者(38%)和标准组未进行辅助化疗的87位(34%)以及标准组进行了辅助化疗的64位患者(34%)。实验组和标准组分别各发生了4例治疗相关死亡(实验组:1例心脏骤停、1例肺栓塞、2例感染并发症;标准组:1例肺栓塞、1例中性粒细胞减少性败血症、1例误吸、1例重度抑郁症导致的自杀)。
综上所述,对于这类患者,该研究实验组所采用的术前化疗相比辅助化疗科降低疾病相关治疗失败的可能性,该实验性疗法或可考虑用作高风险局部晚期直肠癌的新标准疗法。
原始出处:
Renu R Bahadoer, et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): a randomised, open-label, phase 3 trial. The Lancet Oncology. December 07, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
52
#患者预后#
52
#局部晚期#
57
#Oncol#
58
#局部晚期直肠癌#
78
#局部#
49
可以
90
需要更多结直肠癌肝转移的突破
95
顶刊就是不一样,质量很高,内容精彩!学到很多
67
谢谢梅斯分享这么多精彩信息
83