Circulation:急性缺血性卒中/TIA基因多态性和氯吡格雷疗效的荟萃分析
2016-11-05 xing.T MedSci原创
相比于缺血性卒中或TIA接受氯吡格雷治疗的CYP2C19功能缺失等位基因非携带者,CYP2C19功能缺失等位基因携带者有更高的卒中和复合心血管事件发生风险。
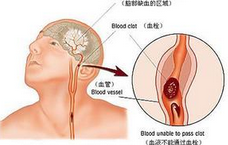
缺血性卒中或短暂脑缺血发作(TIA)患者基因多态性和氯吡格雷疗效之间的关系仍存在争议。近日,心血管领域权威杂志Circulation上发表了一篇来自中国学者进行的一项系统回顾和荟萃分析文章,旨在评估基因多态性,尤其是CYP2C19基因表型,和缺血性卒中或TIA患者氯吡格雷疗效之间的关系。
研究者全面搜索了从PubMed、EMBASE两个数据库成立以来到2016年6月24日期间的数据,纳入了所有有关缺血性卒中或TIA患者接受氯吡格雷治疗和基因多态性的研究。研究的主要终点事件包括卒中、复合血管事件和任何出血事件。
该荟萃分析共有15个研究4762例脑卒中或TIA并接受氯吡格雷治疗的患者,并且他们都是CYP2C19功能缺失等位基因的携带者,相比于CYP2C19功能缺失等位基因非携带者,他们发生卒中的风险明显增加(12% vs 5.8%;风险比为1.92,95%可信区间为1.57-2.35;P<0.001);CYP2C19功能缺失等位基因的携带者复合血管事件的发生也更加频繁(13.7% vs 9.4%;风险比为1.51,95%可信区间为1.10-2.06;P=0.01),然而两组患者出血率相似(2.4% vs. 3.1%;风险比为0.89,95%可信区间为0.58-1.35;P=0.59)。此外,除了CYP2C19基因之外的基因变异与临床结局并不存在相关性。
由此可见,相比于缺血性卒中或TIA接受氯吡格雷治疗的CYP2C19功能缺失等位基因非携带者,CYP2C19功能缺失等位基因携带者有更高的卒中和复合心血管事件发生风险。
原始出处:
Yuesong Pan, et al. Genetic Polymorphisms and Clopidogrel Efficacy for Acute Ischemic Stroke or Transient Ischemic Attack: A Systematic Review and Meta-analysis. Circulation. 2016. http://dx.doi.org/10.1161/CIRCULATIONAHA.116.024913
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#荟萃分析#
60
#缺血性卒#
57
#缺血性#
61
#荟萃#
61
太好了,又学习了。
91
#多态性#
59
对临床治疗有帮助
101