Heart:阵发性房颤患病率和房颤进展的决定因素
2022-07-24 MedSci原创 MedSci原创
阵发性房颤患者房颤进展率为5.5%/年。病情进展的预测指标包括心房重构、性别、二尖瓣反流、腰围以及与凝血状态、炎症、心肌细胞拉伸和动脉粥样硬化相关的生物标志物。
心房颤动通常由阵发性房颤发展为更持久的表现形式。近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员为了改进个体化用药,开发了一种新的阵发性房颤患者房颤进展风险预测模型。

在高凝状态、电生理重构和血管不稳定在房颤进展中的相互作用研究的这项重新评估房颤的中期分析中,研究人员评估了基线时进行广泛表型的阵发性房颤患者,并在随访≥1年期间进行持续心律监测。房颤进展的定义为(1)持续或永久性房颤,或(2)阵发性房颤进展,负担增加3%以上。研究人员通过多变量分析确定了房颤进展的预测因素。
该研究的受试者平均年龄为65(58~71)岁,其中女性为179例(43%)。随访2.2(1.6~2.8)年,417例患者中有51例(5.5%/年)患者出现房颤进展。多变量分析表明,PR间隔、左房功能受损、二尖瓣反流和腰围与房颤进展相关。
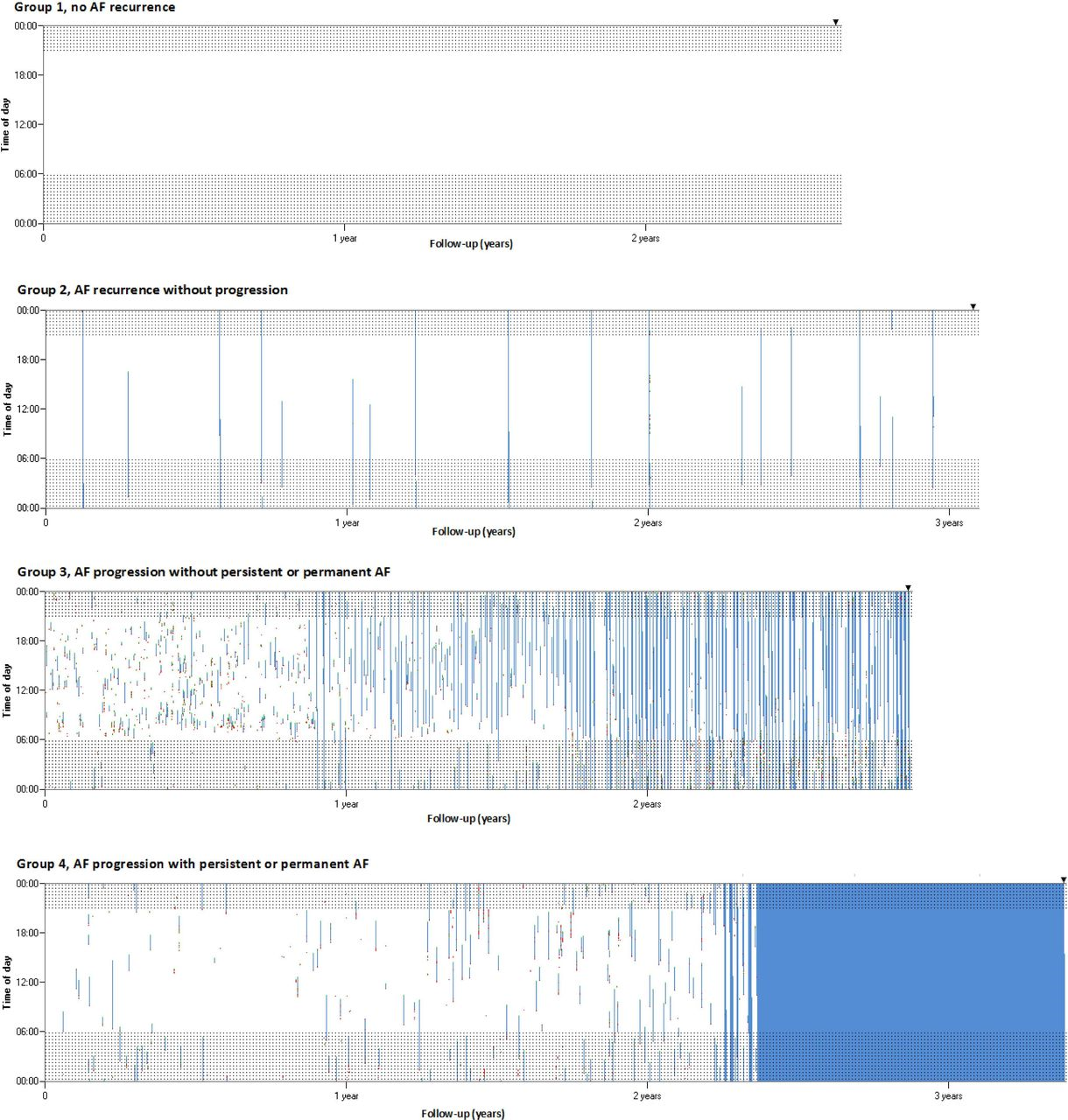
将血液生物标志物纳入模型后改善了模型的预测效能(c值从0.709提高到0.830),并显示男性、较低水平的因子XIIa:C1-酯酶抑制剂和组织因子途径抑制剂、较高水平的脑钠肽前体N末端、蛋白转化酶原枯草杆菌素9和肽聚糖识别蛋白1与房颤进展相关。
由此可见,阵发性房颤患者房颤进展率为5.5%/年。病情进展的预测指标包括心房重构、性别、二尖瓣反流、腰围以及与凝血状态、炎症、心肌细胞拉伸和动脉粥样硬化相关的生物标志物。这些预测模型可能有助于确定房颤进展的风险和治疗目标,但还需要进一步研究进行验证。
原始出处:
Bao-Oanh Nguyen.et al.Prevalence and determinants of atrial fibrillation progression in paroxysmal atrial fibrillation.heart.2022.https://heart.bmj.com/content/early/2022/07/20/heartjnl-2022-321027
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#决定因素#
110
#患病率#
80
#ART#
75
#阵发性房颤#
78
#HEART#
75