TCT 2020丨ULTIMATE研究:血管内超声 vs. 冠状动脉造影指导下植入药物洗脱支架术后3年随访结果
2020-10-19 心关注 心关注
随着介入技术的进步,冠状动脉造影(CAG)是判断冠状动脉病变,判定狭窄程度和介入适应症的金标准。但是,由于斑块常为偏心性或不规则性,CAG仅仅只能显示被造影剂填充的管腔轮廓。
随着介入技术的进步,冠状动脉造影(CAG)是判断冠状动脉病变,判定狭窄程度和介入适应症的金标准。但是,由于斑块常为偏心性或不规则性,CAG仅仅只能显示被造影剂填充的管腔轮廓,故在某些常规投照角度下容易遗漏或低估病变,而且CAG对斑块稳定性的评价极其受限。血管内超声(intravenous ultrasound,IVUS)作为医学超声的一个分支,可利用超声原理探测血管内/血管壁及其周围组织结构,可识别CAG低估的血管病变和识别冠脉易损斑块,还可以指导PCI的治疗策略和评估支架植入效果,因此IVUS在介入心血管病学的发展中扮演着重要角色。
既往的RCT研究和观察性研究提示,在复杂病变(例如CTO、长病变、左主干病变等)和高危患者(ACS)中,IVUS指导药物洗脱支架(DES)植入可以带来临床获益,近几年的荟萃分析也证实了这一点。然而,部分替代终点(比如晚期管腔丢失)的改善是否会转换为临床事件的获益尚存在争议。ULTIMATE研究是一项前瞻性、多中心、随机对照试验,共纳入了1448名接受DES的受试者,并进行为期3年的随访,评估血管内超声与冠脉造影指导下植入药物洗脱支架患者3年的靶血管失败率(TVF)与支架内血栓(ST)发生率。ULTIMATE研究结果证实:IVUS指导DES植入,通过显着降低TVF来改善患者的临床预后,尤其在IVUS评价达理想标准的患者获益更明显,对临床治疗决策起到了重要作用。
研究背景
IVUS是指无创性的超声技术和有创性的导管技术相结合,使用末端连接有超声探针的特殊导管进行的医学成像技术。对于复杂冠状动脉病变,建议选用IVUS指导下植入DES。ULTIMATE研究结果显示:随访1年时,与冠状动脉造影指导下植入DES的患者相比,IVUS指导下植入DES患者的TVF更低。但是,目前尚无IVUS指导下植入DES长期有效性及安全性数据。
研究设计
ULTIMATE研究是一项前瞻性、多中心、随机对照试验,共有1448名接受DES的受试者,按1:1随机分配为IVUS组和冠状动脉造影组,并进行为期3年的随访。主要终点是:随访3年时TVF;安全终点:明确的或可能发生了ST。
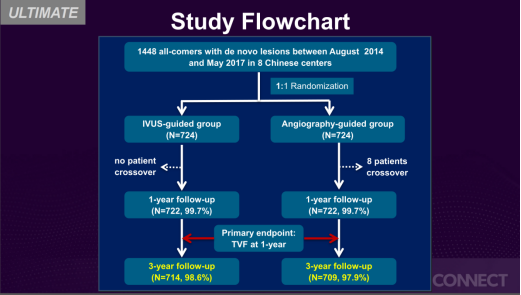
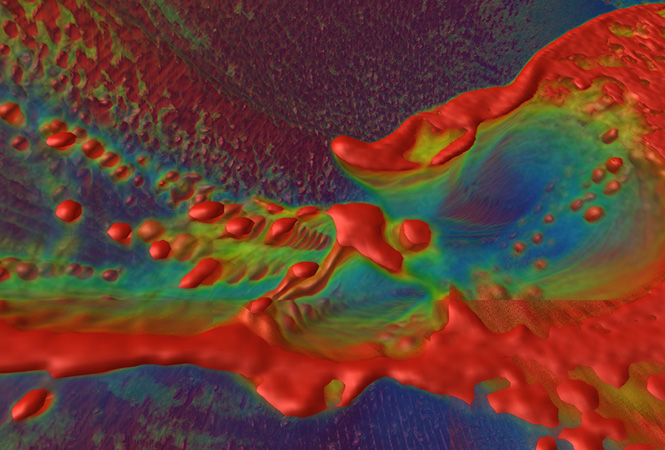
图1. 研究设计流程图
IVUS定义的支架植入的理想标准:
1. 支架段最小管腔横截面积大于5.0 mm2,或达到远端参考管腔横截面积的90%;
2. 支架边缘近端或远端5 mm处的斑块负荷<50%;
3. 无深达中层且长度超过3 mm的边缘夹层。
上述三条标准同时满足才可定义为IVUS达标,若有一条不满足则不能判定为IVUS达标。

图2. 支架植入的理想标准
研究结果

图3. 受试者基线特征资料
主要终点:随访3年时,靶血管失败率(TVF)在IVUS组为6.6%(47例),造影组的TVF为10.7%(76例),两组比较差异具有统计学意义(P=0.01),主要原因可能是与临床驱动的靶血管失败减少有关(4.5% vs. 6.9%,P=0.05)。如图4.1、图4.2所示。
安全终点:明确或可能的ST发生率在IVUS组为0.1%,在冠脉造影指导组为1.1%(P= 0.02)。如图4.1所示。
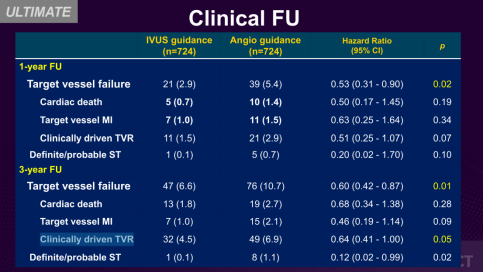
图4.1. 研究结果-主要终点事件
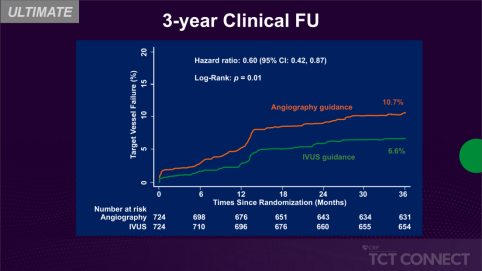
图4.2. 研究结果-主要终点事件
值得注意的是,IVUS定义的最佳手术与次最佳手术相比,随访3年时,最佳手术组的TVF显着减少(4.2% vs. 9.1%,P=0.01)。如图5所示。
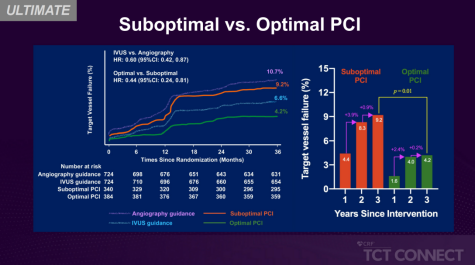
图5. 最佳手术组与次佳手术组比较
研究结论
与冠脉造影指导相比,IVUS指导下的DES植入患者3年随访期间的TVF和ST发生率均显着降低,特别是采用IVUS确定的最佳手术的患者。
团队介绍
天津医科大学总医院是天津市医学中心,综合实力居国内前列。心血管病学专业历经石毓澍、周金台、石嘉玲、万征、孙跃民等几代科主任不懈努力,学术水平始终居国内前列。在现任科主任杨清领导下,目前学科亚专业完备,包括冠心病介入治疗、起搏与电生理、先心病与肺血管病学、高血压和心力衰竭等,各亚专业均在国内有较大学术影响。天津医科大学总医院心内科目前是卫健委心血管疾病心律失常和冠心病介入诊疗培训基地、国家级胸痛中心、国家高血压中心、中国房颤中心、房颤中心示范基地、心内科专科医师培训基地。
点评专家:高玉霞教授
天津医科大学总医院心内科主任医师,医学博士,博士生导师。天津市健康管理协会中老年专业委员会副主任委员、天津医师协会心力衰竭专业委员会常务委员、天津心脏学会女性健康专业委员会常委兼秘书长、主要从事心血管内科的临床医疗、教学和科研工作。擅长疑难心血管疾病的诊断和治疗,尤其是冠心病及冠脉介入治疗、心律失常及术前和术后管理、高血压、心力衰竭及高脂血症的调脂治疗等。研究方向:冠心病和高血压的临床与基础研究,主持并参与科研课题研究多项,其中主持并完成国家自然科学基金面上项目1项,参与天津市科技项目多项。发表学术论文40余篇,其中以第一作者或通讯作者发表SCI论文8篇,曾获天津医科大学科技成果二等奖1项。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#支架术后#
0
#洗脱支架#
81
#随访结果#
67
#支架术#
104
与冠脉造影指导相比,IVUS指导下的DES植入患者3年随访期间的TVF和ST发生率均显着降低,特别是采用IVUS确定的最佳手术的患者。
184
#药物洗脱支架#
124
#TCT#
79
#冠状动脉造影#
83
#造影#
119
#植入#
93